Services

1. What is hirsutism?
Hirsutism is defined as the excessive growth of thick dark hair in an androgen-dependent pattern (male pattern) where hair growth in women is usually minimal or absent like the face, chest, and areolae. It occurs as a result of increased androgen production, increased skin sensitivity to androgens, or both.
2. What causes hirsutism?
Increased androgen levels in females can be due to increased production either by the adrenals or due to an ovarian disease. The ovarian causes for hyperandrogenism are polycystic ovarian syndrome (PCOS) and ovarian tumors. Adrenal causes include Cushing's syndrome, androgen-producing tumors, and congenital adrenal hyperplasia (CAH),.
Other endocrine abnormality that causes hirsutism include hypothyroidism and increased prolactin levels. About 20% of the patients may present with idiopathic hirsutism with normal androgen levels and ovarian function. The cause of increased hair in these women is thought to be related to disorders in peripheral androgen activity. Hirsutism can also occur in some women after menopause. This is due to decrease in ovarian estrogen secretion with continuous androgen production. Hirsutism may be familiar with genetic predisposition or may be related to stress. Many medications can also cause hirsutism.
3. What is the treatment of hirsutism?
Mild hirsutism usually may not require treatment, unless patient is psychologically disturbed. Hirsutism that is associated with irregular menstrual periods or hormonal imbalance requires medical intervention together with cosmetic treatment. Topical cosmetic therapies like Shaving, threading, waxing, using depilatory creams, electrolysis may not be useful in all patients.
Laser hair reduction - Laser hair reduction can treat larger areas, it is painless and no anesthesia is required. Is most effective on dark hairs in fair-skinned people. Multiple treatments may be necessary for long-term hair destruction.


1. What is Alopecia?
Alopecia is defined as a hair-loss disease that affects men, women and children of any age. The onset of the hair-loss is often sudden, random and frequently recurrent. The different types of alopecia based on the type of hair loss includes:
-
Alopecia Areata (AA) - hair loss occurring in patches, usually small and round, anywhere on the body.
-
Alopecia Totalis (AT) - total loss of the hair on the scalp.
-
Alopecia Universalis (AU) - total loss of all hair on the body.
-
Androgenetic Alopecia - male/female pattern baldness.
2. What are the causes for alopecia?
Alopecia areata is an autoimmune condition in which the immune system attacks the hair follicles. People with alopecia areata also have a slightly higher chance of developing other autoimmune diseases such as thyroid disorders, pernicious anemia and vitiligo.
Androgenic alopecia can be caused by a variety of factors related to hormones like thyroid dysfunctions, ovarian cysts, androgen secreting tumors and menopause. Over 20% of people with alopecia have a family member with it and there is some amount of genetic predisposition. Female pattern baldness is caused by hormones (particularly androgens), aging, and genetic predisposition.
Other causes of hair fall include stress, nutritional deficiency, dandruffs, hair dyes, soaps and detergents. Localized trauma to the hair follicles from tight hairstyles like braiding, straightening, ironing, rebounding, tight ponytails and extensions can lead to hair fall. Medications that are used for the treatment of acne, seizures, hypertension, mood disturbance and cancer can also cause hair fall.
3. Will my hair grow back?
The vast majority of people with alopecia experience some degree of re-growth. The chance of regrowth depends upon the cause of hair loss and correction of the precipitating factor. There are various treatments available including topical minoxidil, antiandrogens, supplementation of deficiant vitamins along with local stem cell and growth factor injection.

1. What is Acne?
Acne vulgaris (Pimbles) is skin disease that is characterized by areas of seborrhea (scaly red skin), comedones (follicles impacted and distended by incompletely desquamated keratinocytes and sebum) that may be open (blackheads) or closed (whiteheads). Inflammation leads to papules, pustules, nodules and possibly scarring.
2. What causes acne?
Increase in androgen levels may contribute to the formation of acne. Androgens increase the production of sebum from enlarged sebaceous glands that become blocked and infected with Propionibacterium acnes causing an inflammatory reaction and acne.
Conditions that lead to increased androgen levels like polycystic ovarian disease, adrenal problems, androgen secreting tumor, exogenous androgen intake can lead to acne. Hypothyroidisam is commonly associated with acne. Even with normal androgen levels, acne may be formed as a result of altered sensitivity of the pilosebaceous unit to the circulating androgens.
Stress is commonly blamed for the development of acne. Stress can have many physiologic effects on the body, including changes in hormones that may theoretically lead to acne. In some cases acne lesions can lead to psychological problems such as reduced self-esteem and in very extreme cases, depression.
3. What is the best way to treat acne?
Treatment is case dependent. Your detromatologist will decide the appropriate treatment required. Usually a combination of different treatment modalities is followed depending on the severity of acne and its scarring. The modalities include chemical peels, microderambrasion, derma roller and laser along with appropriate medical management.

1. What is eczema (Dermatitis)?
Eczema is a skin disease caused by inflammation, making the skin itchy and rashy. People with eczema have a weak "outer skin barrier'. This damaged barrier easily loses moisture and lets irritants in, causing dry and itchy skin. Eczema most frequently appears on the face, arms, and legs, but it can show up in other areas, too. Eczema is not contagious.
2. What is Atopic dermatitis (AD)?
Atopic dermatitis (AD) is the most common type of eczema. The general term "eczema" is usually used to refer Atopic dermatitis. The word "atopic" means an allergy that is usually hereditary, and "dermatitis" is defined as inflammation of the skin.
3. What are the signs and symptoms of eczema?
Treatment is case dependent. Your detromatologist will decide the appropriate treatment required. Usually a combination of different treatment modalities is followed depending on the severity of acne and its scarring. The modalities include chemical peels, microderambrasion, derma roller and laser along with appropriate medical management.

1. What is a keloid?
Keloid is a type of scar that is reddish, firm and rubbery. It is benign and noncancerous.
Keloids can develop spanteously or as a result of acne, scratching, trauma or after surgery. They are more common in some sites such as central chest, the back and shoulders and the ear lobes.
2. Are hypertrophic scars different from keloids?
Keloids should not be confused with hypertrophic scars, which are raised scars that do not grow beyond the boundaries of the original wound. Keloids expand in claw-like growths over normal skin.
3. How do you treat keloids?
There are different treatment options available for keloids, however no treatment for keloids is considered to be 100% effective.
-
Silicon sheets / Silicon gel application: It is safe and effective in reducing scars. The earlier the initiation of treatment, the better the prognosis.
-
Steroid injections: Steroid injections into the keloids help to reduce the thickness and itching in the keloids scars. A series of 3-4 injections with triamcinolone acetonide are given every 3-4 weeks. The fibrosis reduces which is evident in the form of softness of the lesion, reduction of size and flattening.
-
Cryosurgery: Cryosurgery is an excellent treatment for keloids which are small and multiple on lightly pigmented skin. It is often combined with monthly cortisone injections. It freezes the skin and causes sludging of the circulation beneath, effectively creating an area of localized frostbite.
-
Surgery: Surgery is done only for depalking the keloids and this will be followed with combination of other modalaties of treatment however regular follow up would be required to prevent recurrence.

1. What is Psoriasis?
Psoriasis is a common, chronic, relapsing/remitting, immune-mediated skin disease characterized by red, scaly patches, papules, and plaques, which are not itchy.
The skin lesions seen in psoriasis may vary in severity from minor localized patches to complete body coverage.
It is genetic disease influenced by environmental factors. It can be triggered by infection, stress, calcium deficiency, smoking, alcohol consumption and certain medicines like oral steroids, non steroidal anti inflammatory drugs, anti hypertensive drugs and anti depression drugs.
2. What are the signs and symptoms?
There are five types of psoriasis: Plaque, guttate, pustular, inverse, and erythrodermic. About 80% of people living with psoriasis have plaque psoriasis, also called "psoriasis vulgaris." Plaque psoriasis causes patches of thick, scaly skin that may be white, silvery or red. These patches can develop anywhere on the skin. The most common areas to find plaques are the elbows, knees, lower back, and scalp.
Psoriasis can also affect the nails. About 50% of people who develop psoriasis see changes in their fingernails and/or toenails. Psoriasis can affect the joints too. Smaller joints of the hand and joints of the knee and lower back can also get involved. If joint pain develops, it is important to consult a dermatologist to prevent joint deterioration.
3. Can psoriasis be cured?
In most patients, it is a chronic, life-long condition with alternating periods of flaring and clearing. There are advanced therapies available and your dermatologist can decide the best treatment option for you.

1. What is urticaria?
Urticaria's is localized itchy, pink wheals (swellings) that may occur singularly or in groups on any part of the skin; they are part of an allergic reaction. Approximately 10-20 percent of the population will have at least one episode in their lifetime. Most episodes of hives disappear quickly in a few days to a few weeks. When hives form around the eyes, lips, or genitals, the tissue may swell excessively. Although frightening, the swelling usually goes away in less than 24 hours. Severe cases of hives may cause difficulty in breathing or swallowing and emergency room care is required.
2. What causes urticaria?
-
Foods : The most common foods that cause urticaria are: nuts, chocolate, shellfish, tomatoes, eggs, berries, and milk. Fresh foods cause hives more often than cooked foods. Food additives and preservatives may also cause hives. Hives may appear within minutes to several hours after eating, depending upon the site within the digestive tract where the food is absorbed.
-
Drugs : Almost any medication can cause hives. Antibiotics, pain medications, sedatives, tranquilizers, diuretics (water pills), diet supplements, antacids, arthritis medication, vitamins, herbal supplements, eye and eardrops, laxatives, vaginal douches, or any other non-prescription item can be a potential cause of urticaria. It is important to inform the dermatologist of ALL prescription and over-the-counter medications being used to help find the cause of the hives.
-
Infections : Many infections can cause urticaria. Viral upper-respiratory tract infections (colds) are a comon cause in children. Other viruses, including hepatitis and a number of bacterial and fungal infections, may cause urticaria.
Most of the patients have coexisting thyroid abnormality. Urticaria can also be manifestation of any systemic illness including malignancy.
3. What is angioedema?
It is a condition characterized by the sudden & temporary appearance of large areas of swelling in the subcutaneous tissue (layer below the skin) or submucosa, with or without hives. In severe cases there can be difficulty in breathing, abdominal pain if the internal organs are involved. This can be life threatening and the patient has to be taken to the hospital immediately.
4. What is the treatment for urticaria?
The best treatment for urticaria is to find and eliminate the cause whenever possible. Antihistamines are prescribed to provide relief and work best if taken on a regular schedule to prevent hives from forming. There are many antihistamines available. No one antihistamine works for everyone. The dermatologist may use combinations to control the urticaria. In severe cases, an injection of epinephrine (adrenalin) may be needed. Cortisone may also bring dramatic relief, but its use must be limited to short periods of time.
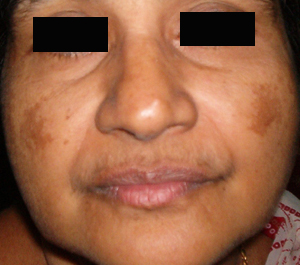
1. What is melasma?
Melasma, also called 'chloasma', is a common skin condition of adults in which light to dark brown or greyish pigmentation develops, mainly on the face. It typically appears on the upper cheeks, upper lip, forehead, and chin but it also can appear on other parts of the body that exposed to sun, such as the forearms and neck. Although it can affect both genders and any race, it is more common in women and people with darker skin-types who live in sunny climates. It is not an infection, it is not contagious and it is not due to an allergy. Also, it is not cancerous and will not change into skin cancer.
2. What causes melasma?
The exact cause is not known, but several factors contribute. These include pregnancy, hormonal drugs such as the contraceptive pill, and very occasionally medical conditions affecting hormone levels. It is so common during pregnancy that some people call it the mask of pregnancy. Some cosmetics that contain perfumes, turmeric, sandal, hair color can increase photo sentivity that increase melasma.
3. What is the treatment for melasma?
Melasma can fade on its own. This often happens when a trigger is causing the melasma, such as a pregnancy or birth control pills. When the woman delivers the baby or stops taking the birth control pills, melasma can fade. Some people, however, have melasma for years or even a lifetime.
If a topical medicine does not get rid of your melasma, cosmetic procedures like chemical peel, microdermabrasion and IPL may succeed, depending on the patient.

1. What is under eye dark circles?
This is a common problem and is frequently described as "tired eyes", where there is a dark discoloration around the eye with or without swelling. They can affect both men and women of all ages.
2. What causes under eye dark circles?
Stress, fatigue, and aging can contribute to the appearance of dark undereye circles. As we age, our skin loses its elasticity and ability to regenerate and as a result, it becomes thinner. This is why more often elderly people will have rather prominent periorbital dark circles regardless of other factors. A variety of medical conditions can also contribute directly or indirectly to the appearance of dark undereye circles. Allergies and asthma lead to itchy, swollen eyes that can be made worse by scratching.
Any medication that dilates blood vessels can affect the skin around the eyes, making the area darker. Undereye circles can be related to thyroid disease, refractive error, iron deficiency, nasal obstruction and sinusitis. Undereye circles sometimes indicate circulatory problems, including kidney and liver malfunction. Nutritional problems, particularly a shortage of vitamin K, and dehydration can also cause these condition.
Dark circles beneath the eyes may be related periorbital hyperpigmentation, which is basically a condition that results in more melanin being produced by the skin below the eyes, resulting in it appearing to be a darker color.
3. How do you treat?
Along with topical depigmentation creams and correction of precipitating factors, Laser resurfacing and Intense Pulsed Light treatments are good options because they can reduce or eliminate the appearance of prominent veins and capillaries. Chemical peels, too, can be effective in rejuvenating skin around the eyes to eliminate dark circles by exfoliating damaged upper layers of skin to reveal new, healthier skin. Also, injectable dermal filler procedures such as collagen injection and fat transfer can be used to augment recessed areas to eliminate the shadowing that can give the appearance of dark undereye circles.

1. What are freckles?
Freckles are flat, tanned circular spots in the skin. The spots are multiple and may develop on sun-exposed skin after repeated exposure to sunlight. These are particularly common in people of fair complexion on upper-body skin areas like the cheeks, nose, arms, and upper shoulders. Freckles are due to an increase in the amount of dark pigment called melanin and are not due to an increase in the total number of pigment-producing cells called melanocytes.
2. How do freckles develop?
Freckles are thought to develop as a result of a combination of genetic tendency (inheritance) and sun exposure.
3. What is the treatment for freckles?
Freckle prevention is mandatory in people with hereditary tendencies. They should start sun protection early in childhood.
Several safe and effective methods are available to help lighten or reduce the appearance of freckles. Frequently, multiple or a combination of treatments may be required for best results. Cryosurgery, Laser treatments, Photo-facials or Intense Pulsed Light may help lighten and decrease the appearance of freckles safely and effectively. Chemical peels can also help lighten freckles and improve irregular pigmentation.

1. What is Vitiligo?
Vitiligo is a skin disorder characterised by white spots in the skin. These spots occur when pigment cells called "melanocytes" are destroyed and the pigment melanin can no longer be produced. Pigment cells are present throughout the skin, hair, mouth, eyes and some part of the nervous system and they can be damaged or destroyed in any of these areas.
2. What is the cause of Vitiligo?
The precise cause of Vitiligo is not known. A combination of genetic, immunological and neurogenic factors is of major importance in most cases. Trauma of any kind (physical, mechanical, chemical, emotional) too can trigger off the disease process. Stress is often implicated as a trigger factor.
Vitiligo affects at least 1% of the population. About 30% of all vitiligo patients say that other family members also have this condition. Even though most people with vitiligo are in good general health, they face a greater risk of having hyperthyroidism or hypothyroidism, vitamin B12 deficiency, Addison's disease (adrenal dysfunction), Alopecia areata (round patches of hair loss) and or uveitis (inflammation with the eyes).
About 50% of all Vitiligo patients develop the disease in childhood/adolescence before the age of 20. Although largely similar to the disease in adults, childhood Vitiligo is a distinct subset of Vitiligo with a higher incidence of family history of autoimmune or endocrine diseases, early or premature greying and poor response too topical PUVA.
3. What is the treatment for freckles?
Freckle prevention is mandatory in people with hereditary tendencies. They should start sun protection early in childhood.
Several safe and effective methods are available to help lighten or reduce the appearance of freckles. Frequently, multiple or a combination of treatments may be required for best results. Cryosurgery, Laser treatments, Photo-facials or Intense Pulsed Light may help lighten and decrease the appearance of freckles safely and effectively. Chemical peels can also help lighten freckles and improve irregular pigmentation.

1. What are warts?
Warts are benign growths in skin that are caused by human papillomavirus (HPV) infection. Wart viruses are contagious. Warts are non cancerous.
2. Who gets warts?
Though any one can get warts, they are common in undernourished children, people with decreased immunity and diabetes mellitus. They are also seen in patients who are on long term steroids or immunotherapy or anti cancer drugs. Warts are more likely to develop on broken skin, such as picked hand nails or areas nicked by shaving, because the virus is able to enter the skin through scratches or cuts.
3. How do dermatologists treat warts?
Some warts will go away without treatment but may take months, or even years, to disappear. In adults, warts may not disappear as easily or as quickly as they do in children. There are many treatments available for warts like cryotherapy, radio frequency ablation and carbon dioxide lasers. The treatment used depends on the patient's age, the type of wart and other comorbid condition. Cryotherapy (freezing) is the most common treatment. It is painless procedure, no local anesthesia is required, may require multiple sitting and there is no scarring. Bleomycin and immunotherapy are also used for resistant warts.
